

In addition, bronchial wall thickening and pleural effusions are found in up to 20% of cases, but they are nonspecific. The ring-shaped appearance is usually groundbreaking here, but this sign can only be found in about 20% of cases with COP. Perilobular pattern regularly accompanied by consolidations and/or GGO in the same lung zone. An abutment of the pleural surface is normal. Margins of these were poorly defined around the interlobular septa. The perilobular pattern exists of bowed or polygonal opacities. Differentiation toward an interlobular septal thickening can occasionally be difficult. The perilobular region is defined by localization in the lobule’s periphery, i.e., in neighboring the interlobular septa. Lower lung lobes predominance helps to differentiate COP from chronic eosinophilic pneumonia, which is usually encountered in the upper lung zones. In the distribution, the peripheral and basal regions are frequently involved, especially along with the bronchial vascular bundles with lobular patterns. Parenchymal consolidations most commonly change their extent and localization throughout the course of the disease. Parenchymal consolidation is the most frequent imaging finding (80-95%), often accompanied by an air bronchogram. Bi-pulmonary, spot-shaped infiltrates with rounded or flat consolidations and accompanying ground-glass opacities (GGO) are common. In COP, usually, no signs of parenchymal destruction are found. This is an important imaging clue to differentiate it from other infectious processes, e.g., bronchopneumonia, which shows a fluctuating or blurred border surrounding normal lung parenchyma.
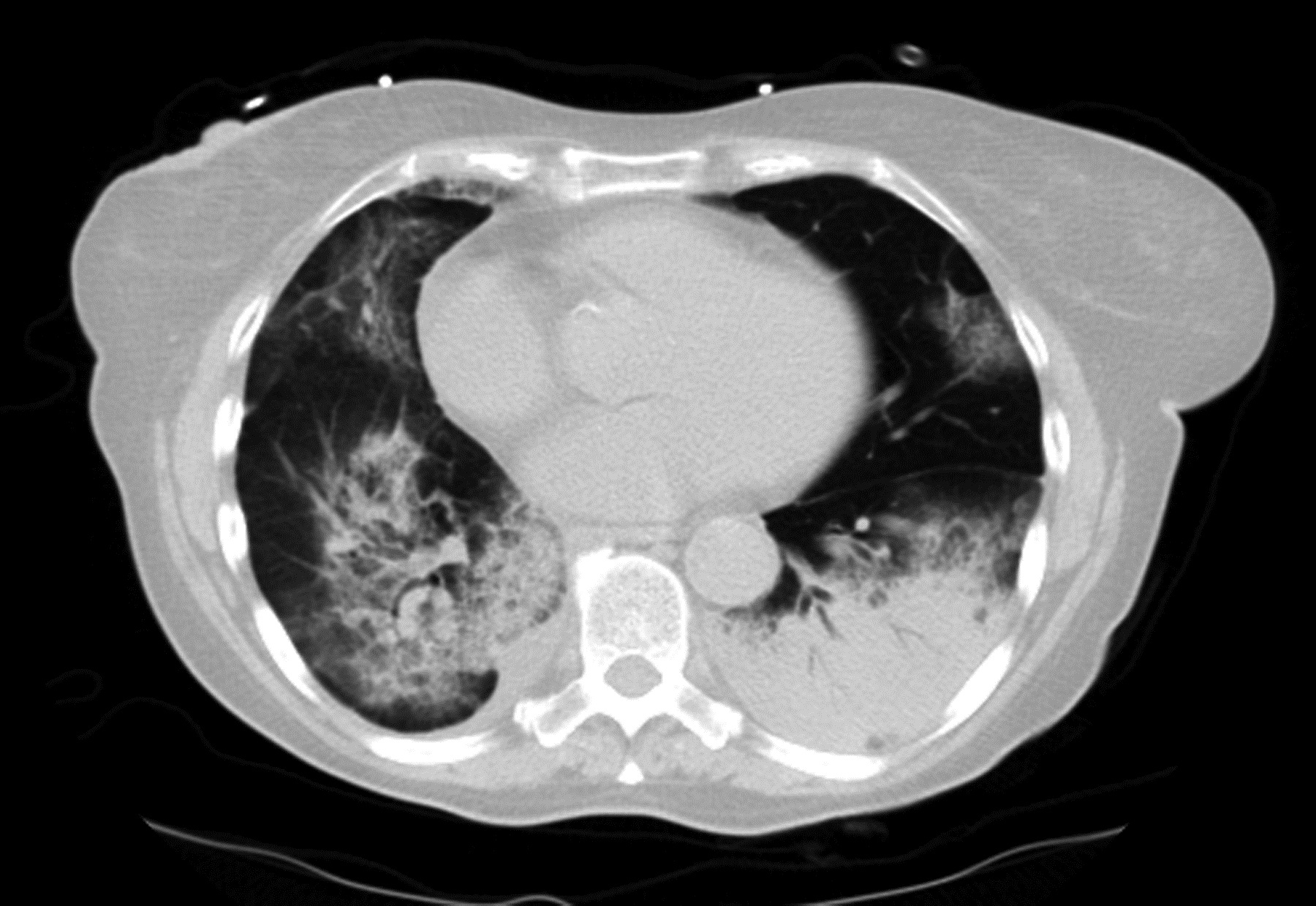
Typically, the COP is sharply delineated from the surrounding parenchyma with a lobular pattern next to the bronchovascular structures. High-resolution computed tomography (HRCT) shows a variety of changes in the COP.

OP: Organizing pneumonia, COP: Cryptogenic organizing pneumonia, HIV: Human immunodeficiency virus, IIP: Idiopathic interstitial pneumonia, DAD: Diffuse alveolar damage, UIP: Usual interstitial pneumoniaįrom a radiological standpoint, COP exhibits different imaging appearances and this review makes radiologists cognizant of the entire spectrum of expected disease findings. The latter may be medically induced, infectious, or associated with vasculitis or malignancy. For practical purposes, differentiation between primary COP without specific etiology and secondary OP is taken. For a better differentiation from the bronchiolitis obliterans syndrome, which is a known, frequent, pulmonary complication of allogeneic stem cell transplantation sometimes accompanying or preceding BOOP, the term COP was preferred in part because this pathology more commonly occurs in other clinical settings. Until the year 2000, the name idiopathic bronchiolitis obliterans with organizing pneumonia (BOOP) was used synonymously. When it arises with no recognizable cause, it is called cryptogenic organizing pneumonia (COP). It usually arises after a recent infection of the peripheral bronchial system, whereby is called secondary OP. Organizing pneumonia (OP) is interstitial pneumonia with an acute or subacute clinical course and a histological pattern compatible with acute lung injury.


 0 kommentar(er)
0 kommentar(er)
